|
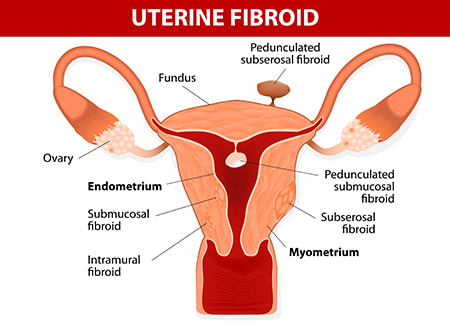
Dr. Gil Wilshire performs an open surgery to remove a fibroid that was causing pain, heavy irregular bleeding, and infertility. The ability to remove these fibroid tumors without damaging the endometrium (cavity) of the uterus is clearly demonstrated.
0 Comments
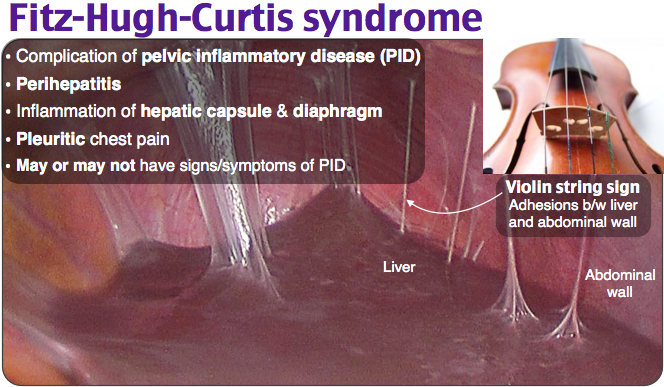
In this video Dr. Wilshire will perform a laparoscopy on a woman in her late 30's, with Fitz Hugh Curtis Syndrome, which caused by a chlamydia infection that goes up through the uterus and tubes and into the abdomen, infecting the entire abdominal cavity.
#STD #Chlamydia #Infertility #CoMo #Missouri #DrGilMD #MissouriFertility
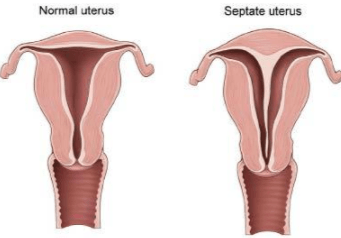
The uterus is normally triangle-shaped and hallow on the inside, with a septum, there is a dip inside, called a septum, and it can cause miscarriages and other reproductive problems. In today's video, Dr. Wilshire performs surgery on a young woman who has a septum in her uterus.
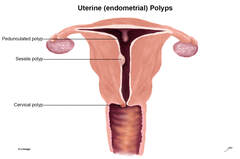
Hello. This is Dr. Wilshire from Missouri Fertility, Columbia, Missouri. Today, we're doing a hysteroscopy on a young woman who has been having abnormal bleeding. She also has polycystic ovarian syndrome. She happens to be from Central America and has a lot of Native American blood. You can see in her overall body shape that she has very thin thighs. She carries her weight in the mid-section, and this makes her at very high risk for growing endometrial polyps. Polyps grow in the uterus when a woman is not having regular ovulation and when she has very high sugar levels and high insulin levels that come from the typical American high-carbohydrate diet. She's been having abnormal bleeding in addition to infertility; so, on ultrasound earlier, we saw a thickened irregular lining of her uterus.
We are looking at her uterus right now with a hysteroscope, and you can see right here that she has some very large polyps, enormous polyps, in the cavity of her uterus. You can see it and we can touch it right now with the forceps. This is a polyp, and if we go past the polyp, there is---yes! Another polyp! No wonder she's been having heavy abnormal bleeding that just won't stop and a lot of cramping. Now, these polyps must come out. They have at least a 5% chance of harboring a cancer, so we are going to take them out. This is the base of this polyp. It probably has a blood vessel and a fibrous base, which means it has been around for a while. You can see how we take these out. We're going to grab the polyp and essentially tear it off the base. It may bleed a little bit, but we should be able to break it free of its connections. We'll do the same thing with the other polyp. After the polyps are removed, we are probably going to make sure her tubes are open with some wires and then she will be able to go home. This is a very quick, safe procedure--hysteroscopy—with very, very low risk. She is under anesthesia, but it is a very light anesthesia called a laryngeal mask, so she won't even have a sore throat when she wakes up—about fifteen minutes from now. This is a hysteroscopy for endometrial polyps, and we are going to get these polyps out. It's probably going to take me a little longer than this video will allow, but you can see how we are going to break off the base and then grab it with a tenaculum. Maybe we can get this polyp out during this video. You can see the base has been broken. We're going to use a little grabber instrument called a tenaculum. Now, this polyp is pretty big, and it may not want to come out through this small opening, but let's see if we can get it for this video. I'm going to twist it, which is called "roping" it up, and let's see if it will come. It may resist. It looks like we may need to clip the base with some scissors, but you get the idea. We are going to get this polyp out, and look at it under the microscope in the pathology department, and if it is cancer, we'll need to see what kind it is and treat her appropriately. Clearly, we need to get these polyps out, because that should stop her excessive bleeding. We will then manage her with carbohydrate restriction, weight loss, and medicines of the progesterone type, and this will get her back to normal, fix her bleeding, and restore her fertility. This is Dr. Wilshire of Missouri Fertility in Columbia, Missouri. I hope that was interesting for you. Thank you very much. In this video Dr. Wilshire discusses the repair of blocked fallopian tubes with Tubal Cannulation surgery. Hello. This is Dr. Wilshire of Missouri Fertility in Columbia, Missouri. Today, we're doing something called a tubal cannulation. Our patient today was told she had blocked fallopian tubes. [She had normal-looking tubes with no history of infection or of severe endometriosis.] She had a laparoscopy a number of months ago, and they were unable to get dye out through the tubes. Today, we're going to see if that is really true. What we are doing is, we are starting out with something called a hysteroscopy. We are looking in her uterus, and we've opened up her uterus with salt water under pressure. We've cleaned out some polyps and some other abnormalities, and now we are able to see the inside of the uterus and the opening of the fallopian tubes. This is the inside of the uterus, called the endometrial cavity, and you can see the openings of both fallopian tubes. There's the left tube, which is on our right, and the right tube, which is on our left. So, now, we are going to take this wire, which is called a urologic Glidewire® (guidewire). We borrowed this wire from the urologists; they use this to remove kidney stones. We are going to put this wire up into this tubal opening that is called the ostium, and…look at that! It passed through a slight obstruction, and you can see the wire going up the tube. I bet you that tube is nicely open now, so we are going to slide the wire out. Fantastic. The right tube is probably open now. And now, we will go over to the left side and perform a similar procedure. There's the opening of the tube, the ostium. We are now going to advance the wire. We've encountered a little obstruction here, so we are going to see if we can get it through, and it does…fantastic! That wire also slides up, so I bet you the left tube is open as well. I'm going to take a picture while I'm here. So, there you have it—that's called a tubal cannulation. Both tubes are now open in this nice woman, and I suspect she will be able to have babies with very little difficulty at this point. Thank you very much. This is Dr. Wilshire of Missouri Fertility in Columbia, Missouri.
Dr. Wilshire discusses surgery for pelvic pain after an ectopic pregnancy. Hello. This is Dr. Wilshire of Missouri Fertility in Columbia, Missouri. Today is obviously a Surgery Day. We have a very interesting case today. Our patient is a young woman who, several months ago, had an ectopic pregnancy. It appears to have been on the right side. Ectopic pregnancies are pregnancies that occur in the body, but outside of the uterus. These can be life-threatening. They are deadly. Nowadays, we can treat them with medicine rather than with surgery most of the time. So, she had her ectopic pregnancy about six months ago. It was treated medically, and she recovered from the pregnancy. Her pregnancy hormone levels are now zero—but now she has pain in her pelvis, and this strongly suggests that she has scar tissue from where this pregnancy used to be. Now, 97% of ectopic pregnancies are in the tube, and almost all of them are around the tube, so we can expect a lot of scar tissue around this tube. We need to evaluate the tube and get her out of pain; these are both very important goals. and we should be able to accomplish both. Of course, some very difficult decision making will need to be made, however—do we save this right tube, can we open it, can we free it of scar tissue, and can we get rid of the issues that might be causing her pain? That's the situation, and that's why we need to go inside. Hopefully, the left tube is open and looks really good. The right tube, however, will almost certainly have scar tissue around it. Now, if we take the right tube out, then she will be forced to use only the one remaining tube to become pregnant. If we leave it in and it is open, then she is at higher risk for having another ectopic pregnancy in this tube. The risk is at least 6% and probably closer to a 25% chance of having another ectopic in that tube. She is aware of this and so is her family. This is a good example of how we can improve anatomy, but we can't make everything perfect again. So, we're going to do the surgery, hopefully help her out, and hopefully not have to make too many difficult decisions. This is Dr. Wilshire of Missouri Fertility. Have a nice day.
Ever wonder what to expect before surgery? Dr. Wilshire and nurse Kim discuss what to expect in a pre-op visit before surgery. Hello. I'm Dr. Gil Wilshire of Missouri Fertility. And I'm Kimberly Ritter, RN, BSN, Surgical Coördinator. G: Today, we're going to be discussing your preoperative preparation. At this point, you've probably had a chat with us about having surgery, we've probably discussed the risks, benefits, and alternatives, and we have all decided that surgery is a good idea for you. Most of our surgeries will be laparoscopic or minimally invasive, so your recovery should be very rapid. Some of you may be having a larger incision and a larger surgery, and obviously your recovery will take a little bit longer, but our standard instructions go something like this—you're going to need a bowel prep. How do you like those bowel preps done, Kim? K: Approximately two days prior to your surgery, we would like for you to get a laxative--magnesium citrate, and drink that the morning of the two days prior to the surgery date. G: So, two days before the surgery, in the morning, you are going to drink this bottle of magnesium citrate. I've heard if you pour it over some ice, it's all right. Maybe a little juice. K: Right. You can put it in the refrigerator, just chill it a little bit, and it's ready to go. This is about an 8 to 10 ounce bottle, sold over the counter at any pharmacy. Just ask the pharmacist and they can help you with that. G: Yes. This bowel prep is not like a bowel prep you would have for a colonoscopy. This is essentially just to get your bowels basically empty. We want you to have a large bowel movement the day before the surgery, so you can come into surgery basically empty, and then you won't have to go to the bathroom for a day or two afterwards either. K: True. Perfectly. And after you consume the magnesium citrate, you can eat lightly that day. G: Yes. Just eat lightly. You don't have to be N.P.O. (which means "nothing by mouth"), but eat lightly the two days before the surgery. Now, the night before the surgery at midnight, what happens, Kim? K: I'd like for you to not eat or drink anything after midnight the night before the surgery. G: Nothing. K: And do not eat or drink anything the morning of your surgery date. G: That's right. You can brush your teeth, but make sure you spit the water out. We want to make sure that you have an empty stomach. Now, the one exception is for medications, I believe. K: If you should have any questions or any concerns, you will be seeing the anesthesiologist and the nurse prior to your surgery, They will call you two days prior to your surgery. G: That's right. They will be telling you what medications you might take the morning of the surgery with a small sip of water; that's okay, and they will be talking to you about that. You might need a blood pressure medicine or a thyroid medicine. There are a few medications they might want you to take, but most of your medications you probably will not take the morning of the surgery. Also, the morning of the surgery, Please take a shower. We want you clean, okay. You don't have to put on fancy make-up or perfume or anything, just come in clean with your teeth brushed. After the surgery, generally what happens, Kim? K: Recovery time after surgery, you can expect four to five days, We will see you back in the office for a post operative visit approximately seven to ten days after your surgery date. G: That's right. After the surgery, we will have what I call a Debriefing Visit. We'll talk about what we found, and we'll talk about future plans, depending on what we found and what we accomplished. Most of our surgeries are minimally invasive, and recovery is generally very rapid, but we generally like for you to take it easy for at least two or three days after the surgery. Many women are able to go back to their normal activities in four to five days, but—as they say--your results may vary. There you go. So, Kim, thank you for your insights. It's wonderful working with you, and I look forward to doing another wonderful surgery, here at Missouri Fertility.
|
�
Archives
March 2023
Categories
All
|
- About Us
-
Services
- Infertility >
- Fertility >
- Third Party Reproduction
- Reproductive Surgery
- Patient Resources >
-
Fertility Facts
>
- Age & Infertility
- Conception 101
- Endocrine Disorders
- Endometriosis
- Fallopian Tube Issues
- Female Infertility
- Infertility FAQs
- Infertility Myths
- Male Infertility
- PCOS
- Pelvic Pain
- Premature Ovarian Failure
- Recurrent Pregnancy Loss
- Secondary Infertility
- Sexually Transmitted Disease
- Unexplained Infertility
- Uterine Disorders
- IVF
- Blog
- Contact
- Patient Portal
|
|
Missouri Fertility
1506 E Broadway Suite 220 Columbia, MO 65201 [email protected] Phone: 573-443-4511 Fax: 573-443-7860 |
Patient Portal |





 RSS Feed
RSS Feed
